- Home
- About Us
- Treatments
- Testimonials
- Media
- International Patient
- Blog
- Cases
- Contact
This information sheet has been given to you to help answer some of the questions you might have about having a rigid cystoscopy. If you have any questions or concerns, please do not hesitate to speak with your doctor or nurse. Piles Doctor in Ahmedabad
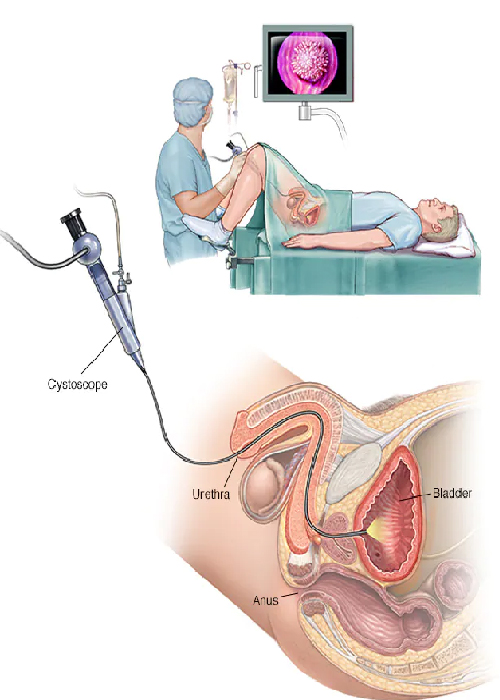
A cystoscopy is a procedure that looks at the bladder and other parts of the urinary system. The the urinary system is made up of the kidneys, ureter (a tube that links the kidney and bladder), bladder and urethra (a tube that urine passes through from the bladder before exiting the body). A cystoscopy involves inserting a special tube, called a cystoscope, into the urethra and then passing it through to the bladder. There are two types of cystoscope: flexible and rigid. A flexible cystoscope is a fiber-optic tube that can move around bends in the urinary system. It is about the thickness of a pencil and is generally used to help make a diagnosis or to see if a treatment has been successful. For your examination, a rigid cystoscope will be used, which is a solid, straight tube with a light at one end. Although both types of cystoscope have side channels where other instruments can be inserted, a greater variety of instruments can be used with the rigid cystoscope. A figure used with kind permission of Health Press Ltd. Reference: Norton A 1999, Patient Pictures Gynaecological Oncology, Health Press Ltd, Oxford The rigid scope is often used to: take biopsies (tissue samples) carry out minor procedures, such as destroying abnormal tissues with heat (diathermy) remove bladder stones or repair bleeding vessels. Piles Doctor in Ahmedabad
Some urinary symptoms, such as those outlined below are due to problems in the bladder or urethra. Sometimes the cause of your symptoms will be clear from X-rays or tests of the blood or urine, but often the only way your doctor can be sure what is going on is to look inside your bladder. A cystoscopy can help to diagnose the causes of symptoms such as: blood in your urine (haematuria) frequent urinary tract infections difficulty or pain when urinating incontinence (inability to control when you urinate) unusual cells found in a urine sample. Piles Doctor in Ahmedabad
Cystoscopies are usually performed with no problems whatsoever. However, there are risks associated with any procedure. Your doctor will explain these risks to you in more detail before asking you to sign a consent form. Please ask questions if you are uncertain. We want to involve you in decisions about your care and treatment. If you decide to go ahead, you will be asked to sign a consent form. This states that you agree to have the treatment and you understand what it involves. If you would like more information about our consent process, please speak to a member of staff caring for you. The specific risks of a cystoscopy include: Bruising and swelling – you may have some bruising and swelling around your urethra from the cystoscope being inserted. This should clear up after a few days. If it does not, please contact us or your GP – you may temporarily need a catheter (narrow tube) placed in your bladder to help drain your urine until the bruising and swelling go down. Damage to the bladder – it is possible to damage or tear (perforate) your bladder with the cystoscope or when taking a biopsy. This can lead to bleeding and infection, which may require further surgery or temporary insertion of a catheter. Please refer to the leaflet, Having a urinary catheter if this applies to you. Bleeding - you may have a small amount of bleeding from the cystoscope being passed up the urethra or from any biopsies taken. Some patients do not have any bleeding at all but some find their urine is slightly pink for a few days after this procedure. Drinking plenty of water (about three liters spaced out over 24 hours) can help to clear your urine. If your urine remains pink after a few days, please contact your GP. Infection – there is a risk that you will develop a urine infection after your cystoscopy, which could result in a fever and pain when you urinate. Drinking plenty of water after the procedure can reduce the likelihood of this. Hernia Surgeon in Ahmedabad
Having a cystoscopy is the only way to diagnose some bladder conditions. Your doctor will discuss any alternatives with you.
You will need to come to a pre-assessment clinic, where you will be seen by a nurse. The nurse will complete some paperwork with you, take some blood tests and check your blood pressure.
You may be admitted to: Day Surgery Unit Surgical Admissions Lounge (SAL) or a urology ward. You may have your rigid cystoscopy in main theatres or the Day Surgery Unit. You should have received a leaflet Surgical Admissions Lounges (SAL) and Day Surgery Units (DSU). Please ask for a copy if you would like one. When you arrive for your procedure, the nurse looking after you will show you around and will complete all the necessary paperwork. She/he will need to monitor your blood pressure, temperature, and pulse and will measure your legs for some special stockings called TEDs. These help to reduce the likelihood of you developing a blood clot in your veins. All patients going for surgery have to wear them. Please make sure that you bring all of your medication with you to the hospital. One of the teams of doctors in charge of your care will visit you before your procedure to ask you to sign your consent form. You will also see an anesthetist who will run through what happens in the anesthetic room with you. You should have been given a leaflet called Having an anesthetic. If you have not received this, please ask a staff member for a copy. You will need to fast before your procedure. Fasting means that you cannot eat or drink anything (except water) for six hours before surgery. We will give you clear instructions when to start fasting. It is important to follow these instructions. If there is food or liquid in your stomach during the anesthetic it could come up to the back of your throat and damage your lungs. On the morning of your procedure, you will be asked to remove all your clothing and change into a gown. For your own comfort, we recommend that you bring your own slippers and dressing gown with you to wear over the top of your theatre gown while you are waiting. The nurse looking after you will run through a special checklist to make sure that you are all ready, and when it is your turn, she will take you to the anesthetic room. After your procedure, you may go back to either the Day Surgery Unit or a urology ward. You will leave hospital from one of these locations once the nurses are happy with your recovery. Please make sure you have someone to take you home as you will not be allowed to leave without a friend or relative accompany you.
You will be given a general anesthetic through a small needle inserted into the back of your hand. This will make you sleep during the procedure, so you will not feel any pain or discomfort. When the cystoscope has been passed into your bladder, the doctor may insert sterile water into help see the lining of your bladder. When the doctor has finished the examination, which generally takes about five to ten minutes, the cystoscope will be gently removed. You will be taken to the recovery unit, where you will stay until you wake up from the anesthetic. Most patients can go home the same evening, as long as they are able to pass urine and their doctor feels they are well enough to go home. However, you may need to stay overnight if you have had a biopsy or required a catheter. If you are well enough to leave hospital on the day of surgery you will need somebody to collect you. Before you leave the hospital, your doctor will prescribe you with painkillers if you want them. You may also be given antibiotics to reduce the risk of infection.
The doctor may be able to tell you the results straight after the procedure. However, if you have had any biopsies taken, these will need to be sent away for testing.
You will be given an outpatient appointment for the following week to discuss the examination and results of any biopsies and whether any further cystoscopy is required. Any results will also be sent to your GP. You will either be given the follow-up appointment before you leave the hospital or it will be sent to you by post. The follow-up appointment will be discussed with you before you leave the hospital.
You might feel dizzy and tired when you go home after the examination. Please rest for the the remainder of the day and the following day to help you recover from the general anesthetic. The anesthetic will take 24 to 48 hours to wear off, although you do not need to stay in bed for this time. Gently moving around your home will help. You may feel a stinging sensation or have difficulty passing urine for the first day or two. You should drink extra fluid for the first 24 hours after the procedure to help with this. If the pain is severe and lasts for more than two days, please contact your GP.
You may want to wear a pad the day after your cystoscopy to protect your clothing from the a small amount of bleeding you may have.
You may be prescribed antibiotics to reduce the risk of infection and it is important that you complete the whole course. You must not drink any alcohol until you have finished the antibiotics and your symptoms have completely cleared. You should also not have sexual Intercourse until any swelling or bleeding has cleared – again, to reduce the risk of infection.
Please do not hesitate to contact the ward if you still have the following symptoms a couple of days after the operation: extreme pain continuous or excessive bleeding passing blood clots a raised temperature of 38oC (100.4F) or greater excessive swelling difficulty passing urine. Please call one of the urology wards for any advice about your operation: Aston Key 0207 188 0709 Florence 0207 188 8818 If you think it is an emergency, please go straight to your nearest A&E department.

User visits the website and navigates to the "Appointment Booking" section.
After completing the form, the user submits their appointment request.
If the requested slot is available, the administrative staff confirms appointment.